Bedwetting is normal in children as they are potty-training and in the pre-school age child. Your health care provider may ask how toilet training is going during yearly visits, but not focus on nighttime dryness until your child is 5 or 6. At this age, 15 out of 100 (15%) still have not achieved dry nights.
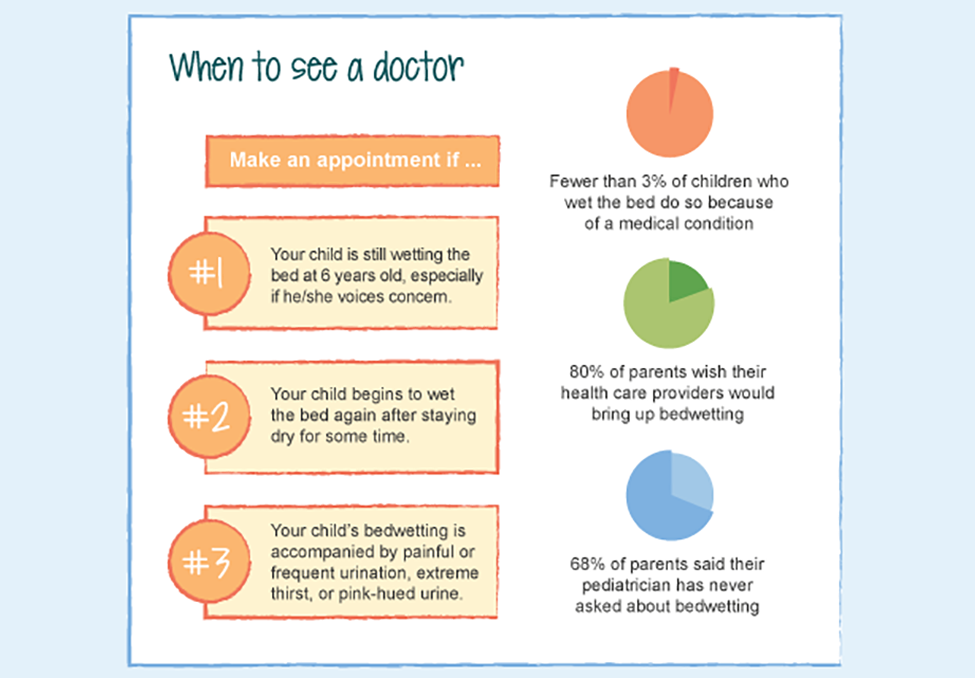
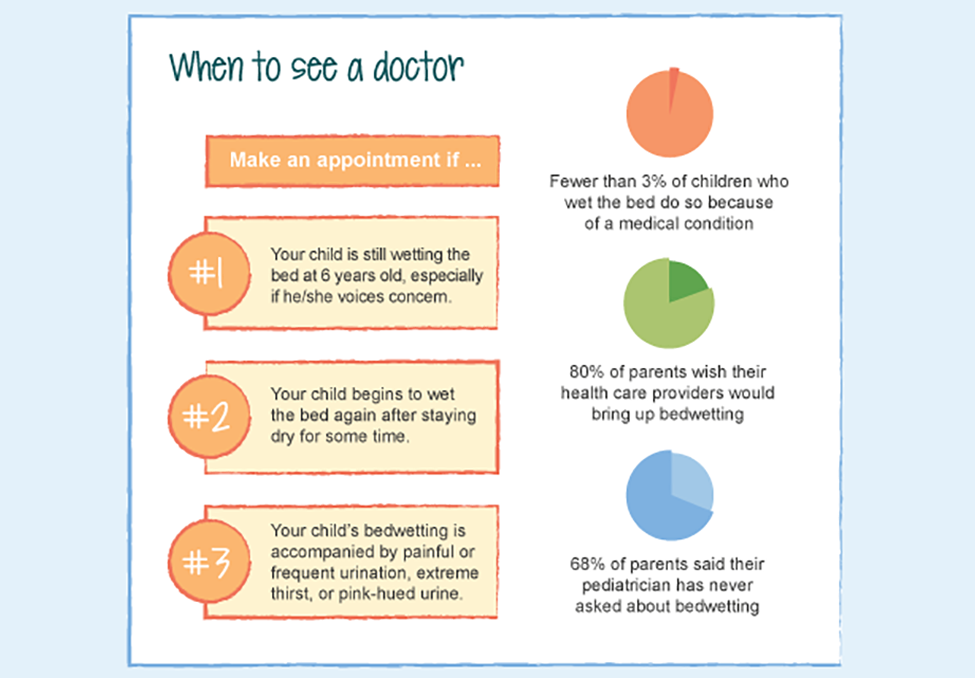
If your child is one of the 15% who have never had a dry night, mention it during your child’s annual check-up, even if your doctor doesn’t ask.
Make a special appointment
- If your child has had 6 months of dry nights, then suddenly starts having nightly accidents, make a special appointment to rule out new medical conditions such as diabetes or urinary tract infections.
- If you notice anything unusual about urination-pain, straining, dark or red color, increased frequency or urgency.
- If you notice a change in stool patterns or if your child has always had difficulty with constipation. Does your child withhold or stain underwear?
Preparing for your visit
Your doctor or nurse practitioner may ask these questions so be prepared with your answers.
- Any medications-any new or seasonal medications, both prescription and OTC, including vitamins and allergy meds, especially if new bedwetting occurred after starting a new medication.
- Family history-genetics play a role in bedwetting; children may stop bedwetting at about the same age as their affected parent.
- Frequency-are there any dry nights, if so, are dry nights becoming more frequent?
- Daytime-any urgency, frequency or leaking noted.
- Any patterns observed-wetting with being overly tired, drinking sugary drinks in the evening, not urinating before bed.
- New bedwetting after more than 6 months of dryness is called secondary enuresis. It may have a more complicated cause.
- Are there any major changes in the family? Is the school setting or virtual learning much different or anxiety provoking?
What they might suggest
Supportive treatment
- Wait-especially if your child is not bothered by wetting and is only 5 or 6
- Move fluids to earlier in the day. Have your child drink more during the day so they aren’t so thirsty after school and in the evening.
- Treat constipation so child has a regular, soft bowel movement most days.
- Wake your child-this is a temporary measure that your child does not learn from, but it usually results in one less urination in the bed. This is tiring for parents and not on the child’s body schedule.
- Medication-usually reserved for older children who have special sleepover situations. Medication does not cure bedwetting; it decreases the urine produced the night it is taken. Bedwetting usually resumes when the medication is stopped.
Curative
Bedwetting Alarm-research proven to be the most effective cure for bedwetting. The alarm sounds when urine is sensed so parents and child know when wetting happens. The child develops the ability to wake up in response to the feeling of a full bladder. This is usually a new, permanent response.